Absorption of Drugs
• Absorption concerns the process of entry of drug in to systemic circulation from site of administration.
•The rate and extent of absorption depend on:
-the environment where the drug is absorbed
-chemical characteristics of drug
-route of administration (which influence bioavailability)
• The route of administration other than intravenous may result in partial absorption and lower bioavailability.
(A) Mechanism of absorption of drug from GIT
• Depending upon their chemical properties , drugs may be absorbed from GI tract by passive diffusion, facilitated diffusion, active transport or endocytosis.
(1) Passive diffusion :
• In this drug move from area of high concentration to area of lower concentration.
- also known as non-ionic diffusion
- The driving force for this process is concentration or electrochemical gradient.
- P.D does not require carrier, is not saturable, and shows low structural specifity.
- The vast majority(about 90%) of drugs are absorbed by this process.
- Water soluble drugs penetrate the C.M through aqeous channels.
- Lipid soluble drugs readily move across most biological membranes due to solubility in the membrane lipid bilayers.
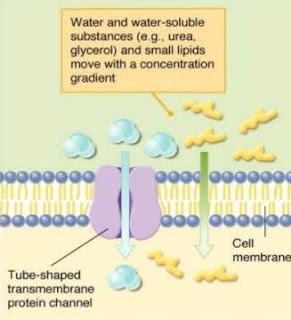
(2) Facilitated diffusion :
• It is the form of carrier transport that does not require expenditure of energy.
- These carrier proteins undergo conformational changes , allowing the passage of drugs or endogenous mollecule into the interior of the cells.
- doesn’t require energy and can be Saturated and may be inhibited by the compounds that compete for the carrier.
(3) Active transport :
• This process require special carrier protein and in this drugs move from lower concentration to high concentration with the expenditure of energy.
- The driving force for this process is ATP.
- capable of moving drugs against concentration gradient.
- Active transport systems are selective and may be compitatively inhibited by other cotransported substances.
(4) Endocytosis and Exocytosis :
• Endocytosis involves engulfment of the drug by the cell membrane and transport into the cell by pinching-off drug filled vesicle.
- This type of absorption used to transport drugs of exceptionally large size across the cell membrane.
- Vitamin B12 transport across gut wall by endocytosis.
• Exocytosis is reverse of endocytosis and many cells used this process to secrete substance out of the cell by pinching off drug filled vessicle.
- Neurotransmitter are stored in intracellular vessicles in the nerve terminal are release by exocytosis.
(B) Factors influencing absorption
(1) Effect of pH on drug absorption :
• Most drugs are either weak acids or weak bases.
•Acidic drugs(HA) release proton (H+), causing an charged anion (A-) to form :
HA <=> (H+) + (A-)
• Weak bases (BH+) can also release an H+. However protonated form of basic drugs is charged and loss of proton produce the uncharged base (B) :
BH+ <=> B + H-
- A drug passes through membrane more readily if it is uncharged.
- thus for the weak acid, the uncharged, protonated HA can permeate through membranes, and A- cannot.
- for a weak base, the uncharged form B penetrates through the cell membrane, but the protanated form BH+ doesnot.
=> Therefore effective concentration of the permeable form of each drug at its absorption site is determined by relative concentration of charged and uncharged ions.
(2) Blood flow to the absorption site :
•The intestine recieve much more blood flow than the stomach so the absorption from intestine is fvoured over stomach.
(3) Total surface area available for absorption :
• With the surface rich in brush borders containing microvilli, the intestine has surface area about 1000 times that of stomach, making absorption of the drug across the intestine more effecient.
(4) Contact time at absorption surface :
• If the drug moves through GI tract very quickly, as can happen with severe diarrhea then it will not well absorbed.
- conversly anything that delay the transport of drug from stomach to the intestine delays the rate of absorption.
- The presence of food in the stomach both dilutes the deug and slows gastric emptying. Therefore a drug taken with meal is generally absorbed more slowly.
(5) Expression of P- glycoprotein :
• It is the transmembrane transporter protein responsible for transporting various mollecule, including drugs, across the cell membrane.
- It is involved in transport of drugs from tissues to blood. Means it pumps the drug out of the cell.
- In area of higher expression, P-glycoprotein reduces drug absorption. In addition to transporying many drugs out of the cells. And it is also associated with multidrug resistance.
(C) BIOAVAILABILITY
• Bioavailability is the rate and extent to which an administered drug reaches systemic circliation.
For Ex: if 100 mg if drug is adminisyered orally and 60 mg is absorbed unchanged , the bioavailabilty is 0.6 or 60%.
- Determinig bioavailability is important for calculating drug dosages for non-intravenous routes of administration.
(i) Determination of B.A :
• It can be done by plotting a graph between plasma drug concentration versus time. One can measure area under curve (AUC), this curve reflect the absorption of the drug. This AUC is compared with AUC of IV injection i.e 100%.
Bioavailabilty = (AUC Oral / AUC of IV) x 100
- Bioavailability of certain routes are :
• Oral, inhalation = 5 to <100
• IV = 100%
• IM, subcutaneous = 75 to <100
• Rectal = 30 to 100%
(ii) Factor that influence the bioavailability :
• Orally administered drugs often undergo first pass metabolism.
- The biotransformation in addition to chemical amd physical characteristics of the drug, determines the rate and extent to which the agent reaches the systemic circulation.
(a) First pass effect :
When the drug is given through enteral route it has to pass through liver via portal circulation and then its enters general circulation so the amount of unchanged drug entering the sytemic circulation decreases, this is referred as first pass effect.
(b) Solibility of the drug : Very hydropholic drugs are poorly absorbed because of the inability to cross the lipid rich cell membrane.
- Paradoxically drugs that are lipophilic are poorly absorbed. b/c they are insoluble in aqeous body fluids and there fore cannot gain the access to the surface if cell.
- for a drug to be readily absorbed, it must ne largely lipophilic, yet have some solubility in aqueous solutions.
(c) Chemical stability : Some drugs such as pencillin G are unstable in the pH of gastric contents. Others such as insulin is destroyed by degradative enzymes in GI tract, which decrese Bioavailability.
(d) Nature of drug formulation : Drug absorption may be altered by factors unrelated to the chemistry of the drug.
For example: particle size, salt form, crystal polymorphism & enteric coating, can influence the ease of dissolution and therefore alter the rate of absorption.
(D) BIOEQUIVALENCE :
• The equivalence of blood concentration of two preparation of same drug, measured over time provided that ghey are given of same route and similar dosage.
- one drug can be safely substituted by other drug b/c both have same bioavailability.
(E)THERAPEUTIC EQUIVALENCE:
• If two similar drugs have comparable efficacy and safety, then they are known to be in the therapeutic equivalence.
- Therapeutic equivalence requires that drug products are bioequivalent and pharmacietically equivalent.











Comments